Breast cancer is a disease in which malignant (cancer) cells form in the tissues of the breast. It is the second most common type of cancer in American women. Breast cancer screening is the process of checking for breast cancer before any symptoms develop. Breast cancer prevention is the action taken to lower the chance of getting breast cancer. Both screening and prevention are important for reducing the burden of breast cancer and improving the chances of successful treatment.
Here are some common Symptoms:
- A new lump or mass in the breast or underarm that feels different from the surrounding tissue
- Changes in the size, shape, or appearance of the breast
- Changes in the skin over the breast, such as dimpling, redness, or pitting
- Changes in the nipple, such as inversion, discharge, or scaling
- Pain in the breast or nipple area.
These symptoms may also be caused by other conditions that are not cancer, so it is important to see a doctor for a proper diagnosis and treatment. Early detection and treatment of breast cancer can improve the chances of survival and quality of life.
Stages of Cancer:
The stages of breast cancer describe how much the cancer has spread in the body. They range from stage 0, which is the earliest stage, to stage IV, which is the most advanced stage. The stages are based on the size and extent of the tumor, the involvement of nearby lymph nodes, and the presence of distant metastases. The stages also take into account other factors, such as the grade, hormone receptor status, and HER2 status of the tumor. The stages help doctors plan the best treatment and estimate the prognosis for each patient. Here is a brief summary of the stages of breast cancer:
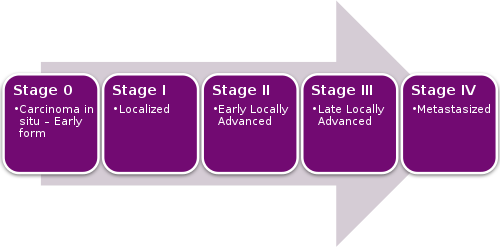
Stage 0
The cancer is confined to the milk ducts or lobules of the breast and has not invaded the surrounding tissue. This is also called carcinoma in situ or noninvasive breast cancer. Treatment may include surgery, radiation, or hormone therapy.
Stage I
The cancer is small (less than 2 cm) and has not spread to the lymph nodes. This is also called invasive breast cancer. Treatment may include surgery, radiation, chemotherapy, hormone therapy, or targeted therapy.
Stage II
The cancer is larger (2 to 5 cm) or has spread to a few nearby lymph nodes. Treatment may include surgery, radiation, chemotherapy, hormone therapy, or targeted therapy.
Stage III
The cancer is large (more than 5 cm) or has spread to many nearby lymph nodes or the chest wall or skin. This is also called locally advanced breast cancer. Treatment may include surgery, radiation, chemotherapy, hormone therapy, or targeted therapy.
Stage IV
The cancer has spread to distant organs, such as the lungs, liver, bones, or brain. This is also called metastatic breast cancer. Treatment may include chemotherapy, hormone therapy, targeted therapy, immunotherapy, or palliative care.
If you want to learn more about the stages of breast cancer, you can talk to your doctor or a cancer specialist for more information.
Breast Cancer Screening
Breast cancer screening can help find breast cancer early, when it is easier to treat. There are different types of breast cancer screening tests, such as:
Mammography
This is an x-ray of the breast that can detect abnormal areas in the breast tissue. Mammography is the most effective way to screen for breast cancer, but it may also have some limitations, such as false positive results (indicating cancer when none is present) or false negative results (missing cancer when it is present). Mammography is less accurate in women with dense breast tissue, who may need additional tests, such as breast ultrasound, 3dimensional mammography, or magnetic resonance imaging (MRI).
Clinical breast examination
This is a physical examination of the breast by a health care professional, who looks for any lumps, changes, or signs of breast cancer. Clinical breast examination may be done as part of a routine checkup or before a mammogram.
Breast Cancer self-examination
This is a personal examination of the breast by the woman herself, who feels for any lumps, changes, or signs of breast cancer. Breast self-examination may help women become familiar with their breasts and notice any changes, but it is not a substitute for mammography or clinical breast examination.
The frequency and age of breast cancer screening may vary depending on the woman’s risk factors, personal preferences, and the recommendations of different medical organizations. Some of the factors that may affect the screening schedule are:
Family history
Women who have a first-degree relative (mother, sister, or daughter) with breast cancer have a higher risk of developing breast cancer themselves, especially if the relative was diagnosed before age 50. Women who have a genetic mutation that increases the risk of breast cancer, such as BRCA1 or BRCA2, also have a higher risk. These women may need to start screening earlier, more often, or with additional tests, such as MRI.

Personal history
Women who have had breast cancer or certain benign breast conditions, such as atypical hyperplasia or lobular carcinoma in situ, have a higher risk of developing breast cancer again. These women may need to follow a different screening schedule than women who have not had these conditions.
Hormone therapy
Women who have used hormone therapy for menopause, especially for more than five years or with a combination of estrogen and progestin, have a slightly increased risk of breast cancer. These women may need to discuss the benefits and risks of hormone therapy and breast cancer screening with their health care provider.
Other factors
Women who have other factors that may increase the risk of breast cancer, such as obesity, alcohol use, physical inactivity, or late age at first pregnancy, may also need to consider their screening options carefully.
Some of the major medical organizations that provide breast cancer screening guidelines are:
The ACS recommends that women with an average risk of breast cancer should have a mammogram every year from age 45 to 54, and then every two years from age 55 and older, as long as they are in good health and expected to live at least 10 more years. Women should also have the option to start annual mammograms from age 40 if they choose to do so. Women with a higher than average risk of breast cancer should talk to their health care provider about when and how often to get screened.
U.S. Preventive Services Task Force (USPSTF)
The USPSTF recommends that women with an average risk of breast cancer should have a mammogram every two years from age 50 to 74. Women in their 40s should make an individual decision about whether to start screening based on their values, preferences, and health history. Women with a higher than average risk of breast cancer should consult their health care provider about the best screening strategy for them⁵.
American College of Obstetricians and Gynecologists (ACOG)
The ACOG recommends that women with an average risk of breast cancer should have a mammogram every year from age 40 to 75, and then every one to two years after age 75, depending on their health status and life expectancy. Women should also have a clinical breast examination every year from age 19 to 39, and then every one to three years from age 40 and older. Women with a higher than average risk of breast cancer should have a mammogram and MRI with contrast every year from age 30 and older, or earlier depending on their risk factors.
Women should talk to their health care provider about which breast cancer screening tests are right for them, and when they should have them. Women should also be aware of the benefits and limitations of each test, and report any changes or symptoms in their breasts to their health care provider as soon as possible.
Breast Cancer Prevention
Breast cancer prevention is action taken to lower the chance of getting breast cancer. By preventing breast cancer, the number of new cases of breast cancer in a group or population is lowered. Breast cancer prevention may include:
Breast Cancer Changing lifestyle or eating habits:
Some lifestyle factors that may help reduce the risk of breast cancer are maintaining a healthy weight, being physically active, limiting alcohol intake, breastfeeding, and avoiding or limiting hormone therapy for menopause.
Avoiding things known to cause cancer:
Some things that are known to cause cancer, such as tobacco smoke, radiation, or certain chemicals, should be avoided or minimized as much as possible. Women who work in occupations that expose them to these carcinogens should follow safety guidelines and wear protective equipment.
Taking medicine to treat a precancerous condition or to keep breast cancer from starting:
Some medicines, such as tamoxifen or raloxifene, may be used to treat women who have a precancerous condition, such as atypical hyperplasia or lobular carcinoma in situ, or to prevent breast cancer in women who have a high risk of developing it. These medicines block the effects of estrogen on breast tissue, which may help prevent the growth of cancer cells. However, these medicines also have some serious side effects, such as blood clots, stroke, or endometrial cancer, and are not suitable for all women. Women who are considering taking these medicines should discuss the benefits and risks with their health care provider.
Breast Cancer Risk-reducing surgery:
Some women who have a very high risk of breast cancer, such as those who have a genetic mutation that increases the risk of breast cancer, may choose to have surgery to remove their breasts (mastectomy) or ovaries (oophorectomy) before cancer develops. This surgery can significantly reduce the risk of breast cancer, but it also has some drawbacks, such as loss of breast function and appearance, early menopause, and psychological distress. Women who are thinking about having this surgery should talk to their health care provider and a genetic counselor about the pros and cons of this option.
Breast cancer prevention is not a guarantee that a woman will not get breast cancer, but it may lower her risk. Different ways to prevent breast cancer are being studied, and more research is needed to find the best ways to prevent this disease. Women should consult their health care provider about their personal risk of breast cancer and the best prevention strategies for them.
To conclude, Breast cancer is a common and serious disease that affects many women. Breast cancer screening and prevention are two ways to reduce the impact of breast cancer and improve the outcomes for women who have it. Women should be informed about the benefits and limitations of each screening and prevention method, and make informed decisions based on their individual risk factors, preferences, and health goals. Women should also be aware of the signs and symptoms of breast cancer, and seek medical attention if they notice any changes in their breasts. Early detection and treatment of breast cancer can save lives and improve the quality of life for affected women
A WordPress Commenter
Thursday 18th of January 2024
Hi, this is a comment. To get started with moderating, editing, and deleting comments, please visit the Comments screen in the dashboard. Commenter avatars come from Gravatar.